Skin Cancer
Skin cancer occurs when DNA becomes irreparably damaged, resulting in the growth of abnormal skin cells capable of invading and destroying surrounding normal skin cells and tissues.
Jump to
Continued definition
As the damaged cells multiply, a visible tumor is typically formed. They are divided into melanoma and non-melanoma skin cancer (basal and squamous cell carcinomas).
Types
& Causes
Skin Cancer
Types of skin cancer
Melanoma


Carcinoma


Carcinoma


Keratosis


Melanoma is a malignancy of the melanocyte, usually darkly pigmented. This is the most dangerous form of skin cancer due to its ability to metastasize and spread to lymph nodes, blood, distant tissues, and organ systems. If detected and treated early while it is still thin, melanoma can typically be cured. If left untreated, the malignancy may grow downward from the skin’s surface and invade healthy tissue. Once it spreads, melanoma can be extremely difficult to treat and often leads to death. Because it is made of pigment producing cells (melanocytes), melanoma is dark in color and may be raised or even with the skin’s surface. Refer to the ABCDEs of melanoma detection chart for examples of characteristics to look for in melanoma. If any mole has any of these characteristics, or is changing in size, shape, color, or texture, the mole should be evaluated by a dermatologist.
Non-melanoma skin cancer is a malignant growth of the epidermal keratinocytes. It typically originates from the squamous cells of the spinous layer (squamous cell carcinoma) or basal layers (basal cell carcinoma) and does not involve melanocytes.
- Basal cell carcinoma (BCC) is the most common form of skin cancer in the US. Presentation can be as simple as a tiny clear or flesh-colored bump, or may be more apparent, such as an open sore or shiny red, pink, brown, or black lesion that could be mistaken for a mole. It is considered the most benign form of skin cancer as it grows the slowest and is the least likely to metastasize. Although BCC rarely spreads to surrounding tissues, making fatality rates exceptionally low, removal can lead to scarring.
- Squamous cell carcinoma (SCC) primarily affects the superficial layers of the epidermis. This type of skin cancer has a red, rough, or flaky appearance and causes thickening of the skin; ulcerations may occur and cause a chronic open sore. Approximately 97% of SCC do not spread; however, if metastasis does occur, scarring, disfigurement, or death is possible.
Actinic keratosis (AK) is considered a pre-skin cancer. It is an abnormal growth resulting from over-exposure to UV rays and, if left untreated, can develop into SCCs. Their appearance is rough and scaly, and they can be tan, red, pink, or flesh- colored. Studies show that up to 60% of squamous cell carcinomas began as actinic keratoses that were never treated. AK can be treated by physicians in several ways, including cryotherapy (freezing), cutterage, photodynamic therapy (PDT), surgical excision, and topical destructive cream medications. Clinical studies have also shown chemical peels, such as Jessner’s solutions and trichloroacetic acid (TCA) preparations, to be effective treatments as well.
ABCDEs of Melanoma Detection

Asymmetry
One half unlike the other

Border
Irregular, blurred, or scalloped

Color
Coloring varies from one area to another or is blue to black
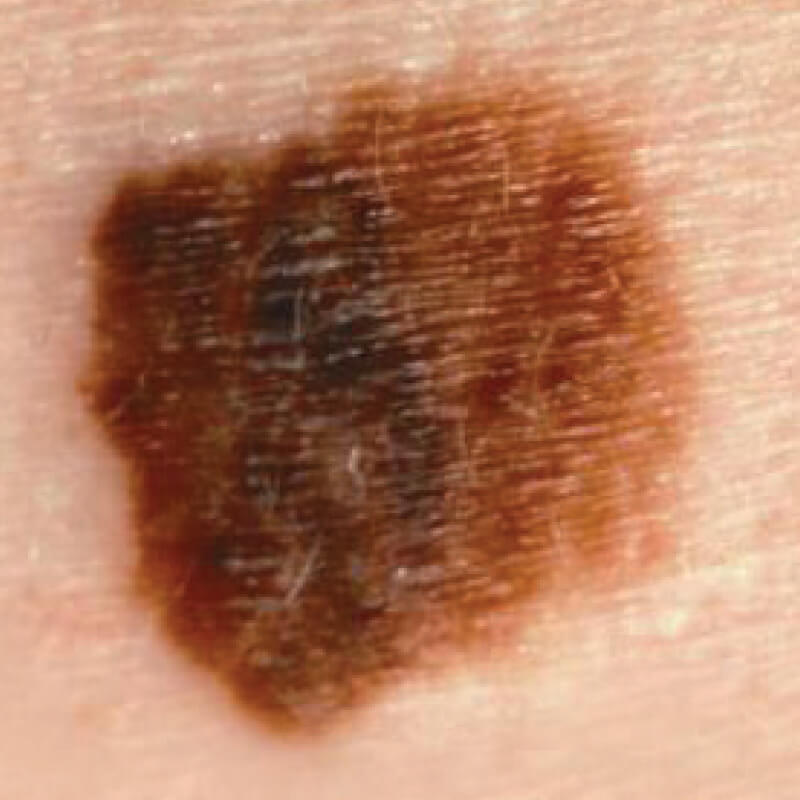
Diameter
Larger than 1/4 inch (the size of a pencil eraser)
Evolution
Any change in size, shape, color, texture, or elevation
Causes of skin cancer
Ultraviolet radiation (UVR) is responsible for 90% of all skin cancers and is the most preventable risk factor for this potentially deadly disease. UVR is broken down into three categories: UVC (200 – 280NM), UVB (280 – 320NM), and UVA (320 – 400NM). The proof of the link between skin cancer and sun exposure dates back to the early 1900s, and as the atmospheric ozone depletes, the number of cases increases each year. UVA rays penetrate deep into the dermis and are responsible for the acceleration of aging (photoaging) associated with sun exposure. UVB radiation primarily affects the epidermis, and is responsible for sunburn and tanning. Both UVA and UVB have been proven to cause DNA damage and mutation, leading to abnormal cell proliferation and cancer. Sun bathing increases this risk significantly.
A tan is the visible result of the melanocyte producing pigment to protect the DNA of the keratinocyte. Upon stimulation from UV rays, the melanocyte transfers packets of pigment (melanosomes) to the keratinocytes throughout the epidermis. The melanosomes are distributed as a cap over the nucleus of the cell where the DNA is stored. DNA damage, induced by UV rays, leads to all forms of skin cancer.
Unfortunately, the frequent erroneous claims regarding the biological need for sun exposure for vitamin D production can be confusing for patients. Although there is no doubt that vitamin D is essential to overall health, adequate amounts can be obtained through food and milk consumption, vitamin supplementation, and through the amount of sun exposure received during normal daily activities, even while wearing sunscreen. The recommended dose of vitamin D for an adult is about 1,000 international units (IU) per day. Additional exposure is never warranted and leads to negative effects, such as accelerated aging, decreased immune function, and skin cancer.
In a survey involving 8,000 Americans, 68% felt that they looked better and healthier with a tan. Unfortunately, this thought process has the use of artificial UV exposure rising steadily each year. Tanning beds are considered even more dangerous than natural sun exposure because of the strength and type of UV rays used. Studies show that 20 minutes in a tanning bed is equivalent to two to three hours of natural sun exposure. In addition, tanning beds use not only high amounts of UVA rays, but also more UVB radiation than currently received from the sun, and even UVC rays which are completely absorbed by the ozone in outdoor exposure. Tanning beds also promote year-round exposure regardless of the season. Undisputable research has linked tanning beds with basal cell, squamous cell, and melanoma skin cancers, and the use of tanning beds is contributing to the staggering skin cancer rates worldwide. The chances of developing melanoma have increased nearly 2,000% in the last 75 years, with nearly 60,000 new cases reported annually. BCC is not only the most common form of skin cancer, but the most common form of cancer in the US. According to skincancer.org, more than 9,500 people in the US are diagnosed with skin cancer every day. More than two people die of the disease every hour. These risks have physicians and scientists comparing tanning bed use to cigarettes and lung cancer, and because of this, strictly enforced regulations are likely to be introduced in the near future. Certain states currently limit the use of tanning beds on those under 18 years of age.
